Novel antibiotic class created
- Published
Scientists have designed a new class of antibiotic which seeks and destroys resistance genes in bacteria.
The unique approach could be used to genetically engineer bacteria in our bodies to become less dangerous.
The technology might also lead to new treatments for metabolic diseases like obesity, the researchers claim.
Scientists and politicians have warned that we face a return to the medical "dark ages" if action is not taken against antibiotic resistance.
The human body houses ten times more bacterial cells than human ones. This community of bacteria is termed the microbiome and its importance in keeping us healthy is increasingly recognised.
One of the problems with current antibiotics is "they hit not only the bad bacteria but also the good bacteria," explained Professor Timothy Lu of the Synthetic Biology Center at Massachusetts Institute of Technology, who led the team carrying out the new research.
"It allows the bad bacteria to flourish."
In a series of laboratory experiments published in Nature Biotechnology, the researchers showed they could produce a molecular "conditional-lethality device" capable of highly targeted action against the "bad" bacteria in a consortium of different strains.
The new antibiotic uses an RNA-guided nuclease called a "Crispr" to hunt down and chop up target genes inside bacterial cells.
"We designed Crispr systems that would go into bacteria and specifically kill only bacteria that contain antibiotic resistance genes or virulence genes," explained Professor Lu.
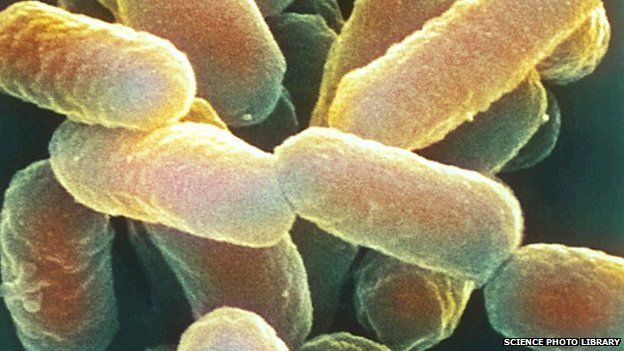
The bacteria targeted in the experiments included a strain of E. coli which can cause severe diarrhoea and kidney failure.
But Professor Lu isn't only interested in killing the deadly bacterium - he wants to rehabilitate it.
In separate experiments the researchers showed they could change the genetic makeup of bacteria without killing them.
"Inherently E. coli is not necessarily a bad organism," Professor Lu explained. "They carry genes that make them bad."
Targeting the bad genes, instead of killing the good and bad bacteria alike, is a new approach which "imposes direct evolutionary pressure at the gene level".
Professor Lu is confident the new antibiotics could be ready for clinical trials in some infections "within a few years."
Resistance is futile?
No new classes of antibiotic have been developed for more than 25 years.
The overuse of available antibiotics favours the survival of bacteria resistant to the drugs. These bacteria can then transmit their resistance genes to other bacteria using tiny circles of DNA called plasmids.
The process effectively speeds up evolution to produce bugs that cannot be killed when they cause disease.
The problem is huge and attracted the attention of Prime Minister David Cameron in July, when he announced a new interdisciplinary panel to address the issue.
"If we fail to act, we are looking at an almost unthinkable scenario where antibiotics no longer work and we are cast back into the dark ages of medicine where treatable infections and injuries will kill once again," he said.
Professor Lu described the problem as "a technological arms race between us and the bacteria".
The new system is "a new type of antimicrobial that really acts very differently to previous ones, and I think that's why we're particularly excited about it," he explained.
The technology could eventually be given to healthy people to prevent antibiotic resistance developing.
"You might take probiotic bacteria while you are healthy, and that probiotic bacteria could distribute these Crispr constructs into your natural bacterial population, and kind of immunise them from being able to pick up bacterial resistance genes.
"So just like the antibiotic resistance plasmids naturally spread in a population, we could potentially design these Crispr constructs to also spread… like a parasite that hops from bacteria to bacteria."
"Think about it like a vaccine - but it's a vaccine for your bacteria, not for you."
Introducing self-replicating gene treatments into the microbiome would not be without risk.
"This is admittedly a little bit radical but I think it's an interesting thing to consider."
'An enabling toolkit'
"The use of antimicrobial agents based on DNA has exciting potential that has not yet been effectively harnessed," said Lucinda Hall, professor of molecular microbiology at Queen Mary University of London.
"The greatest challenge is how to deliver a DNA-based agent into the bacteria to be targeted."
The MIT team explored two approaches to this.
"One idea is that you can just piggy back off the same system that bacteria use to trade resistance genes," Professor Lu explained. In this approach the target cell accepts a 'Trojan horse' plasmid of DNA from another bacteria, with the Crispr hidden inside.
But this would require live bacteria to be given to a patient - so "it is probably not the best solution for an acute infection," he conceded.
Secondly, the team used bacteriophages - natural virus predators of bacteria which are highly adept at injecting DNA into host cells.
This approach is also not without difficulties. "You have to find the right type of phage to bind to each type of bacteria," explained Professor Hall. "There is also a question about how easily phage can reach the site in the body where the bacteria are causing an infection, and whether they will be blocked by antibodies."
"It is something we have to take into consideration," responded Professor Lu. "Other groups have found pretty interesting ways around this, for example coating the bacteriophages with chemicals that basically shield them from the immune system."
Professor Hall was also critical of the bacterial kill rates reported, describing the numbers as "disappointing".
"We need to continue to improve the efficacy," conceded Professor Lu. "But even with [relatively modest] drops in bacterial count you can detect significantly increased survival of the waxworms we were using for testing."
The benefits of manipulating the balance of "good" and "bad" bacteria in the body might extend beyond fighting infection.
"There are certain classes of bacteria in your gut that are known to be overrepresented in people who are obese or have metabolic diseases," explained Professor Lu.
"We could design Crispr-based systems that would go into bacteria, targeted to certain subsets of bacteria, and only activate when they recognise genes that we know are correlated with human disease."
"This is an enabling toolkit for the basic scientists to now start probing these systems a little bit better."
- Published2 July 2014